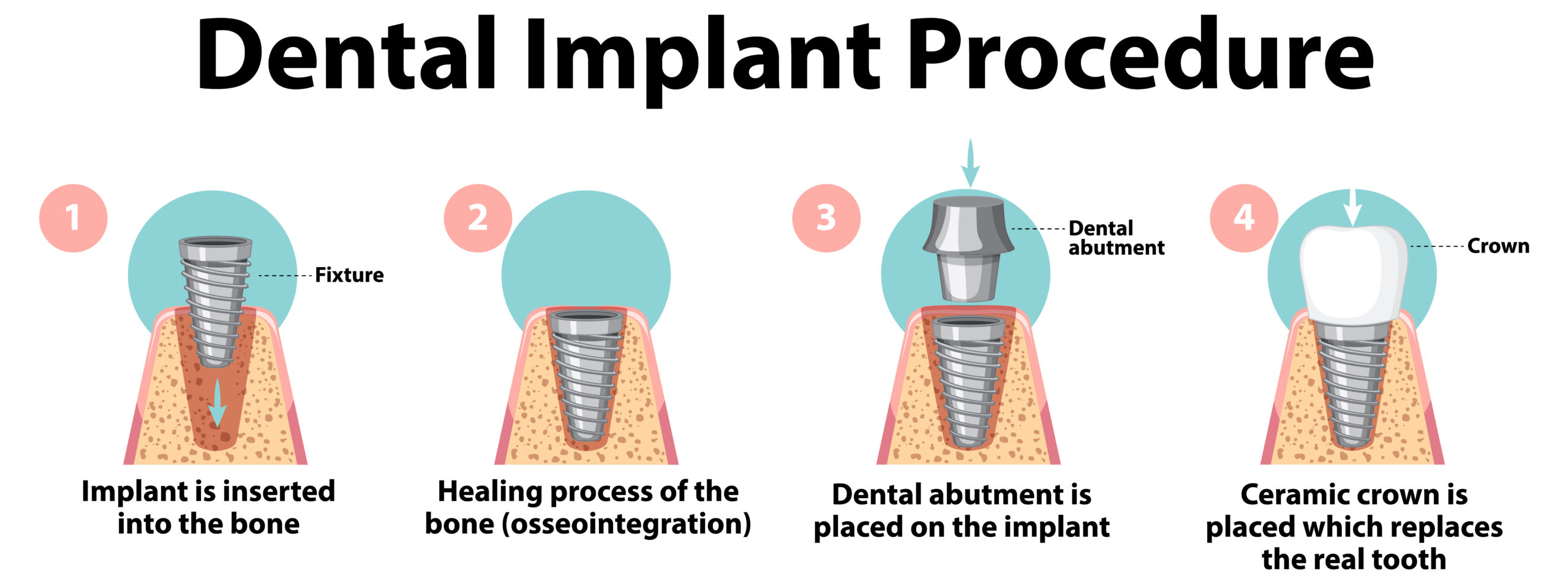
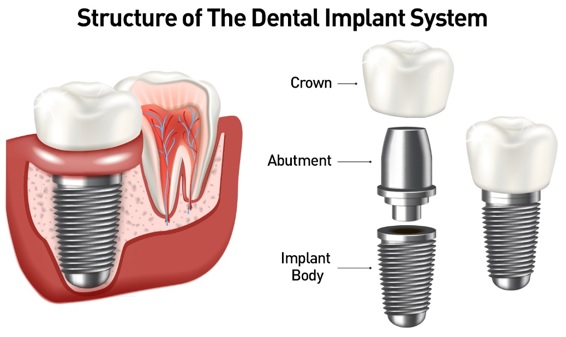
A dental implant is a structure that replaces a missing tooth. With screw-like devices, the surgeon inserts an implant into the jawbone, and it acts as an anchor for an artificial tooth, called a crown.
Dental implants as we know them today were invented in 1952 by a Swedish orthopedic surgeon named Per-Ingvar Brånemark. Today, they are considered the standard of care for prosthetic replacement of missing teeth in dentistry. A dental implant is a surgical fixture that is placed into the jawbone and allowed to fuse with the bone over the span of a few months. The dental implant acts as a replacement for the root of a missing tooth. In turn, this “artificial tooth root” serves to hold a replacement tooth or bridge. Having a dental implant fused to the jawbone is the closest thing to mimicking a natural tooth because it stands on its own without affecting the nearby teeth and has great stability. The process of fusion between the dental implant and jawbone is called “osseointegration.” Most dental implants are made of titanium, which allows them to integrate with bone without being recognized as a foreign object in our body. Over time, technology and science have progressed to greatly improve the outcomes of dental implant placement. Today, the success rate for dental implants is close to 98%.
A device called an abutment connects the artificial tooth to the dental implant.
The crown is custom-made to fit the person’s mouth and match the color of their teeth. Crowns look, feel, and function like natural teeth.
Implants have several advantagesTrusted Source over dentures, which are removable artificial teeth. Implants:
- are more natural and comfortable
- have a higher success rate
- improve chewing function
- lead to a lower risk of cavities developing in nearby teeth
- lead to better maintenance of bone at the site of the lost tooth
- cause decreased sensitivity in nearby teeth
- do not need to be taken out and cleaned every night
However, dental implants are not suitable for everyone. The implanting devices must bond with the jawbone, so a person’s bones must be healthy before they can undergo implant surgery.
Why it’s done
Dental implants are surgically placed in your jawbone, where they serve as the roots of missing teeth. Because the titanium in the implants fuses with your jawbone, the implants won’t slip, make noise or cause bone damage the way fixed bridgework or dentures might. And the materials can’t decay like your own teeth that support regular bridgework can.
In general, dental implants may be right for you if you:
- Have one or more missing teeth
- Have a jawbone that’s reached full growth
- Have adequate bone to secure the implants or are able to have a bone graft
- Have healthy oral tissues
- Don’t have health conditions that will affect bone healing
- Are unable or unwilling to wear dentures
- Want to improve your speech
- Are willing to commit several months to the process
- Don’t smoke tobacco
Background
When a tooth is lost due to injury or disease, a person can experience complications such as rapid bone loss, defective speech, or changes to chewing patterns that result in discomfort. Replacing a lost tooth with a dental implant can significantly improve the patient’s quality of life and health.
Dental implant systems consist of a dental implant body and dental implant abutment and may also include an abutment fixation screw. The dental implant body is surgically inserted in the jawbone in place of the tooth’s root. The dental implant abutment is usually attached to the implant body by the abutment fixation screw and extends through gums into the mouth to support the attached artificial teeth.
Each person is likely to have a different experience of dental implant surgery. Factors that may influence this include:
- the number of teeth requiring replacement
- the location of the implants within the jaw
- the quality and quantity of bone at the implant site
- the person’s underlying oral and systemic health
Depending on these factors, additional procedures may be necessary. These can include:
Sinus augmentation
Placing an implant in the upper jawbone is usually difficult because of the location of the sinuses.
The surgeon may need to perform a sinus augmentation — a procedure to lift the floor of the sinuses to allow more bone to develop so that the implantation can be successful.
Ridge modification
Some people have a jawbone abnormality that prevents enough bone for an implant from developing. In such cases, a surgeon may need to perform a ridge modification.
This involves lifting the gum to expose the area of deformed bone. The surgeon will then use a bone or bone substitute to repair and build up the area. This improves the quality of the jawbone in preparation for dental implant surgery.
What are the types of dental implants? Why are they used?
Historically, there have been two different types of dental implants:
- Endosteal and
- Subperiosteal. Endosteal refers to an implant that is “in the bone,” and subperiosteal refers to an implant that rests on top of the jawbone under the gum tissue. Subperiosteal implants are no longer in use today because of their poor long-term results in comparison to endosteal dental implants.
While the primary function of dental implants is for teeth replacement, there are areas in which implants can assist in other dental procedures. Due to their stability, dental implants can be used to support a removable denture and provide a more secure and comfortable fit. In addition, for orthodontics procedures, dental mini-implants can act as temporary anchorage devices (TAD) to help move teeth to a desired position. These mini-implants are small and temporarily fixed to bone while assisting in anchorage for teeth movement. They are subsequently removed after their function has been served.
For patients who have lost all their teeth due to decay or gum disease of the upper and/or lower arch, an option is available to provide a very stable and comfortable prosthesis using a minimal number of implants. One such is example is the “All-On-4” technique that was named by implant manufacturer Nobel Biocare. This technique gets its name from the idea that four implants can be used to replace all teeth in a single arch (upper or lower). The implants are strategically placed in areas of good strong bone, and a thin denture prosthesis is screwed into place. The All-On-4 technique provides teeth replacement that is stable (not removable) and feels like natural teeth compared to the older method of traditional (removable) complete dentures. Without a doubt, implant dentistry has allowed for more treatment options to replace single and multiple missing teeth with long-term stability and contributes to improved oral health.
After a person has undergone dental implant surgery, they must continue to brush and floss their teeth regularly. Artificial teeth require the same care and maintenance as regular teeth.
The surgeon or dentist will also schedule follow-up visits to monitor the implants and make sure that the teeth and gums are healthy. It is important to return to the dentist every 6 months for professional cleanings.
The cost of dental implant surgery varies, and the following factors can influence it:
- the number and types of implants required
- the location of the implants within the jaw
- whether there is a need for any additional procedures to prepare the mouth for surgery
A dentist or another oral health professional can estimate the cost of dental implant surgery during an initial examination.
Some dental insurance policies cover a larger portion of the cost.
Other tooth replacement options, such as bridges, may be less expensive. However, bridges are harder to keep clean and often require replacement and repair, increasing the overall cost. Dental implants may provide longer-term benefits if a person takes care of them well.
What happens before, during, and after dental implant surgery?

The implant crown is either cemented on or secured with a screw to the abutment.
During the consult and planning stage, the dental surgeon will visually examine the site in the mouth where a dental implant is being considered as well as look at dental imaging studies (X-rays, panoramic films, and/or CT scans). At this time, the quality and quantity of the jawbone are assessed to determine if more bone is needed at the site. Once it has been established that a dental implant can be placed in the desired location, the patient will return for surgical procedures for the dental implant(s). During all surgical procedure appointments, the patient is usually given a local anesthetic to numb the surgical area as well as any other sedatives necessary for comfort and anxiety.
The first stage of oral surgery often involves a tooth or teeth extraction. Oftentimes, the site of a dental implant still has an existing damaged tooth present. In order to prepare for the placement of a dental implant, the tooth will need to be extracted. More often than not, an “alveolar bone graft” (cadaver or synthetic bone) is placed to achieve a solid base of bone for the implant. This site will be allowed to heal for two to six months. For a site that has no tooth and bone loss is present, it will require a different bone graft that is placed on top of the existing jawbone (“onlay bone graft”). This procedure is more involved and usually requires about six or more months of healing. In some instances, when enough bone is present, the damaged tooth can be extracted followed by the implant placement procedure at the same appointment. This procedure is called “immediate implant” placement.
In the situation where an implant is to be placed in the maxilla (upper jaw) in the back or posterior region, sometimes the available amount of bone may be limited by the presence of the maxillary sinus (air-filled space found in the bones of the face). “Sinus augmentation” or “sinus lift” is performed to raise the sinus floor and graft more bone into the sinus. This will make more bone available to support a dental implant.
Once the adequate, strong bone is present, the site is ready for the implant. At the implant placement appointment, the dental implant (titanium post) is placed into the bone with a special drill and tools. A “healing cap” is placed over the implant, the gum is stitched up, and the healing phase begins. During this healing phase, a temporary denture can be made to replace missing teeth for esthetic purposes. Healing time depends greatly on the quality of bone present. Healing time is usually anywhere from two to six months. During this time, the implant becomes integrated with the bone. It’s important to avoid placing any force or stress on the dental implant as it heals. Follow-up appointments to check the surgical site are typically done to ensure that no infection exists and healing is taking place.
After the required healing period, the dental implant is tested to determine whether it was successfully taken up by the surrounding bone. Once this has been confirmed, a prosthetic component is connected to the dental implant via a screw. This component is called an “abutment.” It will serve to hold the replacement tooth or “crown.” The dentist will take an impression (mold) of this abutment in the mouth and have the implant crown custom-made to fit. The implant crown is either cemented on or secured with a screw to the abutment.
Dental implants can significantly improve the quality of life and the health of a person who needs them. However, complications may sometimes occur. Complications can occur soon after dental implant placement or much later. Some complications result in implant failure (usually defined as implant looseness or loss). Implant failure can result in the need for another surgical procedure to fix or replace the implant system.
Benefits of Dental Implant Systems:
- Restores the ability to chew
- Restores cosmetic appearance
- Helps keep the jawbone from shrinking due to bone loss
- Preserves the health of the surrounding bone and gums
- Helps keep adjacent (nearby) teeth stable
- Improves quality of life
Risks Associated with Dental Implant Systems:
- Damage to surrounding natural teeth during implant placement
- Injury to the surrounding tissues during surgery, such as sinus perforation
- Injury during surgery (for example, fracture of surrounding jawbone)
- Inadequate function, such as feeling like the teeth do not bite together normally
- A sensation that the tooth is loose or twisting in place resulting from an abutment screw loosening
- Implant body failure (looseness of the implant body)
- due to systemic infection, which may be more likely in patients with uncontrolled diabetes
- due to local infection in bone and gums supporting the implant body
- due to delayed healing, which may be more likely in patients who smoke
- Difficulty cleaning the gums around the implant, resulting in poor oral hygiene
- Untreated periodontal disease
- Post-surgical numbness due to nerve impingement or damage
- Always notify health care providers and imaging technicians that you have dental implants before any magnetic resonance imaging (MRI) or x-ray procedures. Dental implants can distort or interfere with these images. FDA is not aware of any adverse events reported for MRI or x-ray procedures with dental implants.